Integrated Photonics Spotlight: Advancing Healthcare and Biomedical Applications Through Non-Invasive Glucose Monitoring
26 August 2025How InnoPIC’s Photonic Raman Spectroscopy Platform Is Taking Aim at One of Medicine’s Most Elusive Challenges.
Diabetes affects over half a billion people globally. That’s more than the populations of the United States, Brazil, and Japan combined, dealing with a chronic condition that demands round-the-clock monitoring. And for millions of them, managing blood sugar isn’t just a matter of taking medication; it’s about tracking the ever-fluctuating tides of glucose, day and night, with a needle or sensor in the skin.
This invasive method is not flawless, and it often misses the most dangerous spikes or crashes. The load on patients is physical, mental, and emotional. But until today, the technology to make this process smooth, pleasant, and exact has been difficult to find. One of the most remarkable submissions in the recently concluded PhotonDelta Global Photonic Engineering Contest was a groundbreaking concept that has the potential to shake up the healthcare and biomedical fields.
The Netherlands-based initiative, InnoPIC, is striving to develop a non-invasive, continuous glucose monitor (CGM), widely regarded as the pinnacle of digital health. Their method combines photonic integrated circuits, Raman spectroscopy, advanced signal conditioning, and AI analytics to create a new type of wearable biosensor for healthcare and biomedical uses. If it scales, it won’t just disrupt how diabetes is managed; it could fundamentally reshape how we interact with our biology.
The Pain Point in Healthcare: Invasive Monitoring and Missed Spikes
Finger-prick glucose tests have been a mainstay for decades. However, they come with significant limitations, both literal and figurative. They require routine, manual effort and only offer snapshot data. They miss post-meal spikes, nocturnal decreases, and stress-induced changes that can cause neuropathy, renal illness, and cardiovascular difficulties.
Despite improvements, modern invasive CGMs use filament-based sensors under the skin. These systems provide better data but are expensive, irritable, and need frequent replacements. Their reliance on subcutaneous tissue readings also introduces latency in glucose detection.
With millions of diabetes cases yearly, the healthcare industry is under pressure to improve monitoring accuracy, invasiveness, and accessibility. A continuous blood sugar monitor without puncturing the skin or disrupting daily life is desirable.
That’s the unmet need InnoPIC is aiming to solve with integrated photonics.
A Photonics-Based Approach: InnoPIC’s Vision for Glucose Monitoring Without Needles
Many biosensors use Raman spectroscopy, an optical method that identifies molecules by light scattering. Glucose contains a distinctive spectral fingerprint. For non-invasive glucose monitoring, Raman is ideal. Unfortunately, its signal, especially from human skin, is generally too weak, noisy, and unpredictable for real-time tracking.
That’s where InnoPIC’s innovation could begin. Their proposed wearable CGM system doesn’t rely on drawing blood or accessing interstitial fluid. Instead, in their concept, it sends a regulated beam of light onto the skin and gathers the faint Raman-scattered light that bounces back, which may show glucose levels at the molecular level.
However, collecting this data is only the first challenge. The real trick is making sense of it. InnoPIC suggests tackling the weak signal problem using single-photon avalanche diodes (SPADs), specialised detectors capable of registering single-photon events with ultra-high sensitivity. These detectors could significantly enhance the Raman signal without requiring high optical power, keeping the system safe for continuous skin contact.
Layered on top of this hardware is a proposed noise reduction protocol and an AI-driven algorithm. The software would filter out background noise, isolate meaningful Raman shifts, and interpret the data into glucose values in real time. Combined, the optical and digital systems form a complete, integrated photonic solution, aimed squarely at delivering the world’s first commercial-grade, non-invasive CGM.
Inside the Tech: Materials, Platform, and Architectural Choices
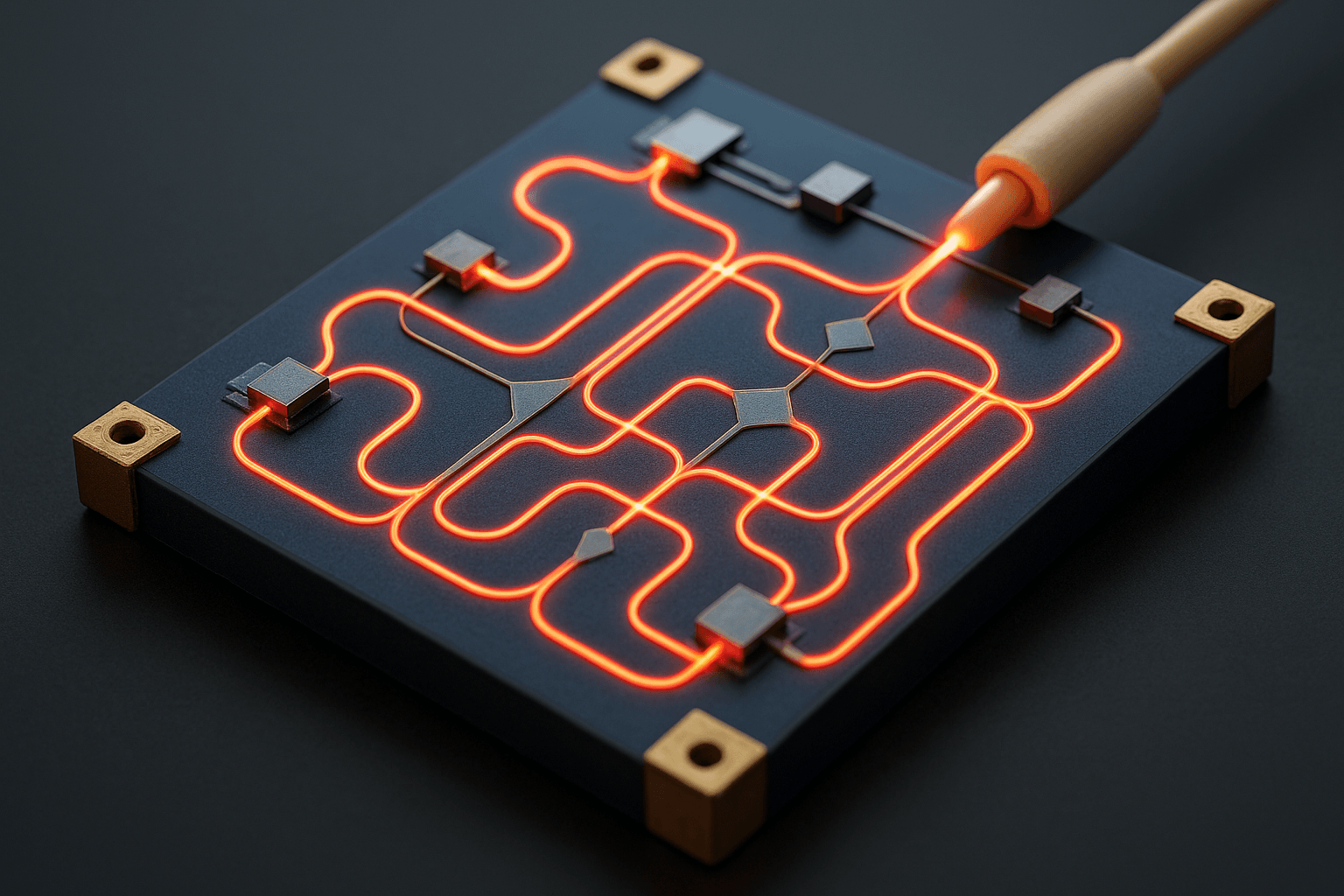
To realise this concept, InnoPIC is exploring AIM Photonics’ silicon nitride (SiN) platform and its TLX component library. SiN was selected for its optical properties, specifically its low fluorescence and excellent transmission in the near-infrared spectrum, which is ideal for Raman-based biological sensing.
Biomedical photonics faces fluorescence challenges. Illuminated biological tissues emit background light that can overpower Raman signals. Ultra-low intrinsic fluorescence in SiN could reduce this interference, resulting in better spectral readings with greater signal-to-noise ratios.
The device’s architecture consists of a tightly integrated photonic circuit, where light from a laser source is routed through waveguides toward the skin-facing Raman interface. SPADs detect photons, which can travel back through the same waveguide that delivered the laser or through separate collection channels built into the circuit.
Then, it digitises these optical signals and feeds them to a machine learning algorithm that aims to correlate Raman characteristics with glucose concentrations. Early simulations and modeling imply that better detection and AI-driven analytics could detect variation within clinically meaningful tolerances.
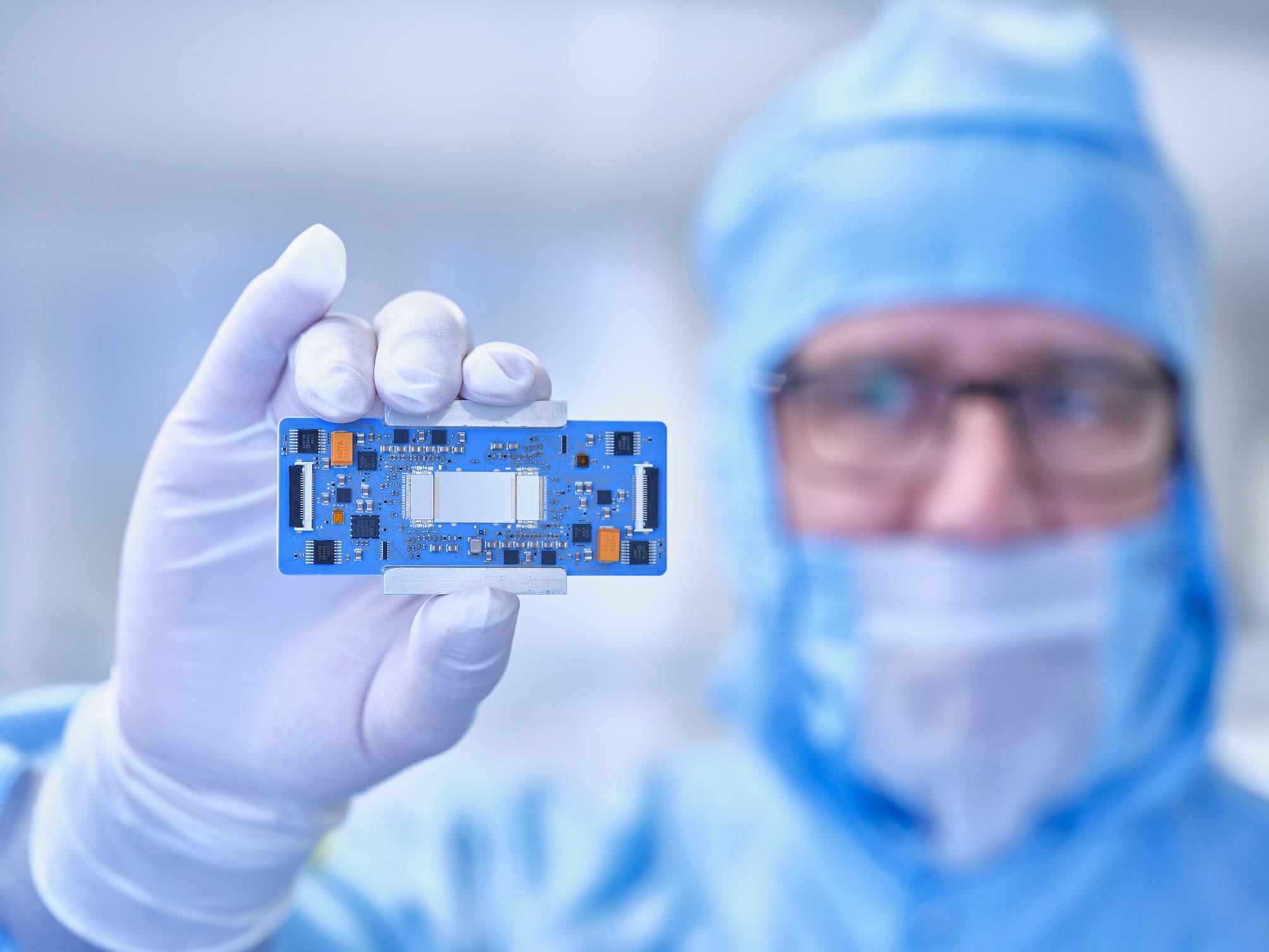
As the concept matures, the team is also exploring potential migration to IMEC’s silicon photonics process design kits (PDKs). These kits offer even lower propagation loss and better support for integrated electronics, which is crucial for the development of future wearable form factors. The ability to print scalable PICs with foundry-grade precision will be essential as the project moves from concept to functional prototype.
System Design and Photonic Flow
In InnoPIC’s system, light and data paths are carefully routed from source to sensor. A miniaturised on-chip laser generates a coherent light source directed through SiN waveguides. This light is projected onto the skin via an external interface or lens embedded within a wearable device, likely in a smartwatch or patch configuration.
Once the light interacts with skin tissue, a portion of it is inelastically scattered—producing the distinct Raman effect. This scattered light, containing the glucose spectral signature, is captured and guided back into the PIC. The system would use wavelength-specific filters to separate Raman shifts from the original excitation signal and other biological noise.
SPADs positioned after the Raman filters in the optical path detect these faint signals and initiate a photon-counting process. Due to their ultra-fast response times and ability to register single-photon events, SPADs are ideal for interpreting the minimal light levels characteristic of skin-based Raman.
The embedded signal conditioning algorithms are intended to process the raw optical data in real time, reducing background noise, compensating for skin variability, and standardising the readings. The AI algorithm would then translate the clean signal into meaningful glucose values, displayed to the user on a connected app or wearable interface.
High Risk, High Reward: Why InnoPIC Calls This a Moonshot
InnoPIC’s concept sits at the edge of what’s technically feasible, balancing between genuine breakthrough and the real risk of failure. The crew readily admits it is a high-risk, high-reward project. The goal is to create the first scalable, noninvasive CGM to compete with needle-based treatments.
However, the roadmap is complex. The team must prove that the optical and computational system can reliably connect Raman signals with blood glucose levels across skin types, ambient conditions, and use situations.
Miniaturization is another. While elegant on paper, the current platform must be condensed into a compact, power-efficient package suitable for continuous wear. Integrating lasers, SPADs, waveguides, and signal processing into a palm-sized or wrist-mounted form factor will require advances in photonic packaging and hybrid integration.
Then, there are regulators. After a thorough clinical evaluation, the FDA (or EMA) must approve medical-grade CGM systems. Certification is time-consuming and data-intensive. InnoPIC will also need silicon photonics-savvy manufacturing partners to grow production while ensuring biocompatibility and dependability.
Still, the potential payoff is staggering. The global market for CGMs is valued at tens of billions and is growing annually. A non-invasive solution that eliminates current systems’ pain, cost, and friction could command massive consumer interest, insurance adoption, and public health value.
Healthcare Impact: Disruption Potential Across Diagnostics and Personal Medicine
While the primary application is diabetes, InnoPIC’s technology has far-reaching ramifications, such as detecting dehydration, monitoring lactic acid during exercise, or measuring ketones in dietary management. The capacity to non-invasively monitor biological molecules enables several real-time diagnoses.
Imagine wearable sensors that could identify dehydration before symptoms appear, lactic acid changes during athletic performance, or ketogenic diet and fasting ketone levels. Optical Raman-based measurements of many of these biomarkers are possible if signal quality and interpretation models are refined.
In the long term, platforms like InnoPIC could become the foundation of “skin-based labs,” sensors embedded into clothing, watches, or patches that quietly monitor dozens of health metrics simultaneously. This would empower preventive care and personal medicine at a scale never before possible.
It also holds particular promise for underserved populations. These wearables could offer high-quality diagnostics to remote clinics, rural communities, and mobile health networks in areas without hospitals or labs. This democratization of monitoring could reshape global health delivery models.
Conclusion: A Future Where Monitoring Meets Comfort
Patients with diabetes have long endured discomfort, vigilance, and compromise. However, integrated photonics, signal detection, and AI may enable painless, precise, and continuous health monitoring.
InnoPIC’s PhotonDelta Global Photonic Engineering Contest entry shows the courage needed to advance healthcare innovation. It combines foundational research with practical ambition to rewire how we comprehend, manage, and interact with our bodies.
There is still much work ahead. But if the light scattered from our skin can reveal the stories of our glucose levels—without blood, without pain, without pause—it’s not just a technological breakthrough. It’s a redefinition of comfort, control, and care in modern medicine.